L.A'.s first street psychiatrist makes his sidewalk rounds, transforming homeless lives

For the record:
10:42 a.m. Sept. 13, 2022: A previous version of this article said the Los Angeles district attorney sits on a committee that reviews requests to initiate conservatorships. The D.A. sits on County Counsel.
Before she met Dr. Shayan Rab, Diana Silveria was the daughter of Elvis Presley, hanging out with Lynyrd Skynyrd on a skid row sidewalk.
Three weeks later, Silveria, 51, was taking medication and slowly coming to reality in a room at the Russ, a single-room-occupancy hotel.
Under Rab's care she was beginning to piece together shards of memories — from her childhood in California to her mother's phone number. She had agreed to Rab's plan to move, once she'd fully stabilized, into long-term residential treatment away from the mayhem of the streets she'd been living on.
If the plan holds, Silveria's picture may go up beside some 30 others on a gallery of success stories pinned to a wall in the county outreach office on 6th Street in the heart of skid row.

A psychiatrist with the Los Angeles County Department of Mental Health, Rab leads a small but growing initiative in street-based treatment that is beginning to make inroads into the population of homeless people who wander L.A.'s streets with untreated mental illness.
They practice an emerging specialty of psychiatry that has been gaining momentum over the past decade but is still rare in street medicine programs around the country.
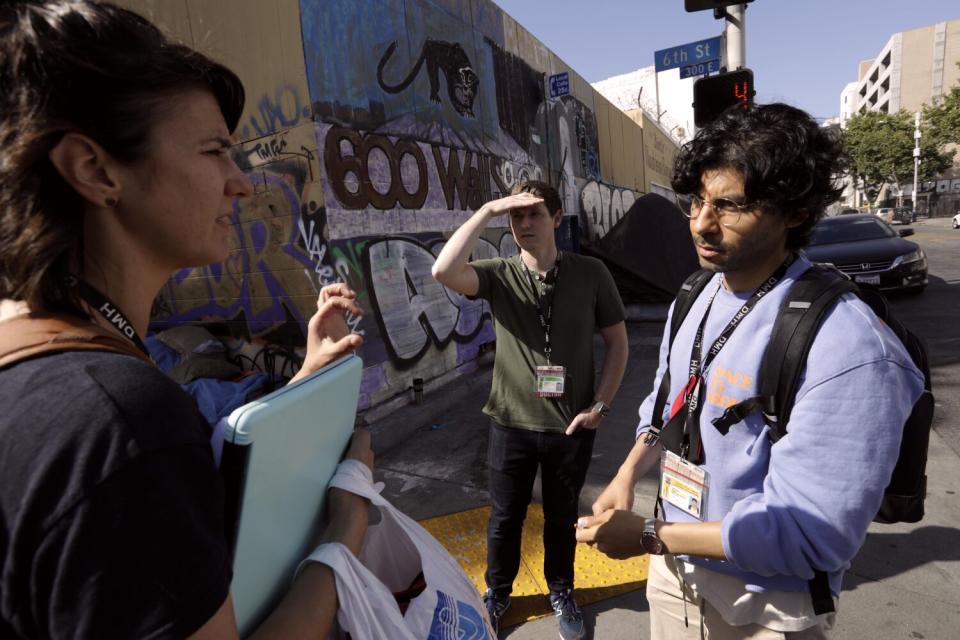
Rab and four other psychiatrists and two psychiatric nurse practitioners are attached to the teams of outreach workers, social workers, nurses and substance abuse counselors of the county's Homeless Outreach and Mobile Engagement (HOME) program. They treat clients where they find them and are using innovative techniques to manage people averse to treatment, including conducting court hearings on the sidewalk.
The team is still being expanded, with HOME budgeted for at least eight psychiatrists.
"You are seeing two different versions of the patient. When we work with an individual on the street we see how an individual is living in the community, what the realities of their environment are like."
Dr. Shayan Rab, psychiatrist with L.A. County Department of Mental Health
At full strength, it would be the nation's most robust street psychiatry program, if it's not already, said Katherine Koh, who has been practicing street psychiatry since 2018 with the Boston Healthcare for the Homeless Program and Massachusetts General Hospital.
"That's wonderful," Koh said. "I would argue that few populations bear greater psychological burden than homeless people yet given the magnitude, there are very few resources for treating them."
Street psychiatry is a radical departure from practicing in a traditional setting.

"To target people who experience chronic homelessness, we must immerse ourselves into their lives and penetrate that bubble," said Atlanta-based social worker Franco Bejarano, writing for Social Worker Today. "We are not going to do that sitting behind a desk, inside an office, asking a person with mental illness to maneuver public transportation across town, requiring them to keep an appointment."
Rab and his colleagues work in filth, noise and disorder treating mental illness that is often compounded by poor health, physical injury, developmental disability, trauma and substance abuse.
Rab works comfortably in that unpredictable environment. The wiry 37-year-old, who mixes music in his spare time, sports long curly locks, bicycles the short commute from his downtown home and faces the chaotic scenes of skid row with a constant smile.
He joined the Department of Mental Health in 2016 after earning a medical degree from USC and completing his psychiatric residency at Olive View-UCLA Medical Center in Sylmar. Three years later he became its first street psychiatrist, in charge of putting together the team.
It has taken Rab three years to build his model, fitting psychiatry into the complex networks of outreach, housing and medicine that is the Los Angeles homeless services system.
Working with Olive View, he now welcomes residents on his calls, showing them the side of patients' lives not seen in the emergency rooms and outpatient clinics where traditional psychiatry is learned.
"You are seeing two different versions of the patient," Rab said. "When we work with an individual on the street we see how an individual is living in the community, what the realities of their environment are like."
They also see the result of what Rab calls revolving treatment that begins with a 72-hour involuntary hold in an ER. By law, hospitals must arrange a place for homeless patients to live after discharge. The most readily available placements are in shelters where the patient is guaranteed food and a bed.
"In a clinical setting, when someone says they want to go back to the shelter I didn't know what that looks like," Rab said. "Now that I have the perspective of the street, it looks like nothing is going to happen. A discharge to shelter has no structure, especially an individual dealing with severe mental health condition. They need more structure."
Without follow-up psychiatric care, medication prescribed in the ER wears off, leading to a quick return to the streets and eventually a new commitment.

Rab's model seeks to stop that cycle using interim housing — preferably in single-occupancy rooms like those at the Russ — as a first stop where his clients can stabilize on medication while he works with them toward what he calls a clinical endpoint.
That could be a family member's home, an apartment with support services, a board and care home or a locked psychiatric residence, all depending on how well the client responds to medication.
Rab breaks the work into phases that engage all members of the HOME team.
"It begins with outreach," he said. "That's where the social workers and the community workers who are skilled at making initial interactions build the foundation of the relationship."
They help with food and clothing, work to obtain government benefits and search for shelter beds.
"The goal is to get an individual indoors as quickly as possible and then help them understand how to self manage their medication which is not too easy in the streets, but if we move them indoors it's a lot easier," Rab said.
Most critically, it makes it easier for the team to find their patient.
"To target people who experience chronic homelessness, we must immerse ourselves into their lives and penetrate that bubble."
Franco Bejarano, Atlanta-based social worker
But with no manual to guide them on the streets, Rab and his team have to improvise what would normally be basic tasks like obtaining laboratory tests and administering medication.
"Whatever the standard of care was in a regular clinic, I had to incorporate it somehow and modify it for the streets," he said.
There's no stockroom for medication. Instead, a nurse makes runs to the pharmacy to fill Rab's prescriptions.
"Because we are doing medication support, it often requires that we are seeing our clients daily," he said..
To place his clients in residential institutions, Rab must screen them medically.
"You have no idea how many barriers there can be to entry," he said. "Traditionally [the system is] designed for individuals coming out of hospitals. We're doing placements from the street directly. We don't have the structure of the hospital to get all the meds, to get all the labs quickly."
A HOME team nurse goes to the client to draw samples and carries them to the lab.
All the while, Rab must navigate the maze of county bureaucracy in search of treatment beds that, for the indigent, are routinely overbooked.

At the Beverly Hills Senior Care in Mid-Wilshire, Rab drops by a couple of times a month to check in on almost a dozen clients he has there. Initially, the visits are to smooth their transition from his care to a private doctor. Over time, they blend into social calls.

"Are you taking all your medication?" he asked Frances Mae Jones on a recent afternoon, as she sat in a wheelchair beside her sleeping roommate.
"Yeah, I have trouble sleeping sometime," Jones said.
Rab told her he would talk to her doctor about adjusting the medication.
In clipped answers to a series of questions, Jones said someone drove her to Los Angeles from Jacksonville, Fla., and dropped her on a downtown street about 16 months ago. She was happy with the board and care but was planning to move on, she said.
Then Jones began moving her lips as if speaking to herself. Rab decided it was time to call off the interview. He did not want to over-agitate her.
It had taken three months of persuasion to get Jones to leave the street, Rab said. It was not likely she would be able to leave the board and care soon, if ever, even though she is not being held involuntarily.
"You can't just head out of here," he said. "You have to come up with a plan."
The mission of street psychiatry necessarily strikes a tenuous balance between public pressure to address the untreated mental illness evident on the city's streets and the slow, uncertain course of any one person's treatment.
Success is measured in weeks or months, is never guaranteed and can always be undone.

On a recent outing Rab walked with Karla Bennett, the supervising social worker on the team, three blocks west to Spring Street, a bustling mélange of hipsters, tourists, business people and homeless wandering out of skid row. There they found Juan Luna at his usual spot, standing on the sidewalk in urine-soaked sweatpants with a plastic sheet around his shoulders like a poncho on a summer day.
Rab opened a notebook and drew three lines on a blank page, one column for social history, one for medical history and one for family history. It's his own method to bring discipline to interviews that can be brief, chaotic and overlain by sirens and ambient sounds of human distress.
He started with routine questions:
Age? "26." They knew he was at least twice that.
Where did he sleep? "L.A. Mission." They knew he slept on the sidewalk.
"Do you want me to get you clothes?" Rab asked.

"No, I'm fine," Luna said.
"I took you to the Weingart, did you like that?" Bennett asked, referring to a large homeless services agency on skid row.
"Weingart, yeah."
"We want to get you back there," Bennett said.
In fact, they did not think he would go. In their three-month attempt to treat Luna, they had committed him on an involuntary hold at Gateway Hospital, the first time he was off the streets in months. He did well there and agreed to a step-down to the Weingart Center.
"But he only lasted a month or two inside and then he kind of wandered back to his old spot," Bennett said.
When Luna appeared to become disengaged, Rab and Bennett left him where he stood and later discussed their next move. Unlike Silveria, Luna had not responded well to treatment and medication. He agrees to go to the shelter but then changes his mind.
Rab said he was considering a conservatorship, the legal proceeding that places a person found to be gravely disabled under the protective care of another person, possibly a relative, but in a case such as Luna's, usually the county public guardian.

Ideally, someone like Luna would start on the conservatorship path after a stay in a psychiatric hospital followed by a commitment to a locked facility where he would stay through court proceedings that can take months. That's rare, though, because hospital staff are reluctant to petition the court, even after repeated 72-hour commitments, in part because of the cost and scarcity of treatment beds in longer-term facilities called institutions for the mentally disabled.
"That is the ultimate funnel point and has the slowest turnaround," Rab said. "If you are in line for an IMD it can be a very long wait."
Rab and his fellow street psychiatrists are blazing an alternate path called outpatient conservatorship. From start to finish, it occurs on the street. When their clients have court dates, they no longer have to appear in person. Instead, Rab finds them at their street haunts and conducts the hearing over a video connection to the court on a laptop computer.
To start that process for Luna, Rab would have to present the case to the Outpatient Conservatorship committee, a group representing agencies including the Department of Mental Health, County Counsel, the public defender's office and the public guardian.
Requests for conservatorship are infrequent. HOME team psychiatrists recommended conservatorships for 78 clients over the past two years, less than one for every 40 clients they worked with. Of those, 50 have been placed in conservatorship. The committee rejected 10 and the remainder are in process.
That pace is certain to grow as more psychiatrists come on board, said Connie Draxler, acting chief deputy director for the Department of Mental Health. Already the pilot has far exceeded its modest goal of five conservatorships.
"We were not sure the pilot would even be successful," Draxler said. "We found over the course of the year, we were able to overcome a lot of anticipated barriers and found that we could make this a component of our regular program."
But it can be a tool only for a certain type of individual. Despite political pressures to wield conservatorships to get homeless people off the streets, pushing them into court-ordered treatment is the last resort, she said.

"If a client is willing to get into treatment, accept housing, any alternatives where the HOME team can address food, clothing and shelter, we don't want them conserved."
Most of Rab's cases follow the course of Silveria's treatment: building a relationship, starting medication, persuading her to try interim housing and, hopefully, finding a permanent home away from skid row. In her case, if a family reunion is not possible, she could be placed in subsidized housing. Most of his clients can't make that jump so quickly and are placed in board and care homes, licensed facilities with 24-hour supervision, food services and medication management, as a first step.
Because of the strict protections for medical privacy, there is little data to gauge how much of an impact street psychiatry is having on untreated mental illness. The Department of Mental Health discloses no information about individual clients. Unlike arrests by law enforcement, involuntary mental health detentions, as well as placements that result from them, are not public records.
The Times accompanied Rab and Bennett for two days in late May and early June under a first-of-its-kind protocol that required each client they observed to sign a privacy waiver before the reporter and photographer could approach. A new waiver was required for each contact with a client.
As a gauge of the initiative's overall impact, the county provided The Times with summary data covering more than 53,000 HOME team interactions with people on the street in 2020 and 2021. About half of those were casual contacts with people who were not yet clients.
For each of the 3,418 people who became clients last year, team psychiatrists, case managers, nurses and social workers made an average of eight calls, five times for case management and three times for mental health services. The teams responded to crises 625 times to execute an involuntary commitment or calm someone in a crisis.

With all this, there's still no doubt that Rab's work has barely scratched the surface of the tragedy on L.A.'s streets. While the number of mentally ill homeless people has never been reliably counted, experts figure it could run into the tens of thousands. He estimates that he has had about 200 clients over his three years in street psychiatry. Some have reunited with families, some are in board and care homes, some interim housing and some still on the street.
"Not all of them are successful," he said. "People just get lost."
He takes on six to seven new cases a month, and his active caseload averages 40 to 50.
A recent study by the California Policy Lab at UCLA found that about 10% of the people living on the street — about 4,500 in the City of Los Angeles — had a clinical diagnosis of severe mental illness such as schizophrenia or bipolar disorder.
That number would rise significantly under a broader view of mental illness.
Koh, the Boston psychiatrist, includes alcohol and drug use disorders, depression and personality disorders as conditions needing psychiatric care, a definition she said could encompass up to three-fourths of homeless people, citing a recent compilation of studies.
"I think there is a tremendous burden of suffering that comes with anxiety disorders and personality disorders," Koh said.
As Rab's psychiatric team grows, the number of people drawn into treatment and stable housing will undoubtedly increase.
But it will always be a slog, one patient at a time, with privacy laws preventing a glimpse of the overall progress.
Two months after The Times last saw Luna in his plastic poncho, based on the advice of the county counsel, the Department of Mental Health released a statement on his status:
"The L.A. County Department of Mental Health is well aware of Juan’s whereabouts and safe living situation. Apart from this update, DMH cannot legally provide any further information on Juan."


Silveria, who had moved into the Beverly Hills Senior Care, the board and care home Rab frequently uses, agreed to another interview.
She seemed like a different person. The hair color and makeup were gone along with the stress that had infused her demeanor at the Russ. She recalled her childhood in Sacramento — without Elvis — and said she had talked to her mother. She talked excitedly about going to the beach.
Asked if she considered the board and care home, she did not hesitate.
"No, I'm going to bail as soon as I get better," she said.
Rab reminded her that this was a stepping stone and that he was working on a permanent home.
In a frenetic conversation, Silveria talked about becoming a movie star and asked Rab if he could get her some makeup.
He promised he would.
This story originally appeared in Los Angeles Times.

