Could treatments for rare diseases be found in neighborhood pharmacies? New uses for old drugs offer promise

When computer scientist Matthew Might was trying to find a treatment for his son Bertrand, he used his digital skills to simulate how 200,000 drugs might act on a genetic mutation that had left the boy with seizures, developmental delays and, oddly, an inability to cry tears.
It appeared 70 of the drugs might have some benefit, 15 were already approved for use in the U.S., and one worked in a lab model of the genetic fluke.
That one turned out to be the antacid Prevacid, and soon after he started giving it to Bertrand his seizures improved. A second drug, used to treat osteoarthritis and inflammatory bowel disease, allowed the boy to cry real tears for the first time.
The drugs ultimately couldn’t save Bertrand’s life. He died last year shortly before his 13th birthday.
CHOOSING HOPE
The fourth in an occasional series exploring how scientific advances are transforming care for rare diseases.
But it showed the power of using already-approved drugs to treat rare disease.
The simple concept has been used many times before.
Viagra, the erectile dysfunction drug, originally was developed to treat hypertension. The morning sickness treatment thalidomide, famously taken off the market when it caused horrible birth defects, was resurrected as a therapy for multiple myeloma and leprosy. Remdesivir, intended to treat Ebola, was effective at treating patients hospitalized with COVID-19.
Even if these drugs hadn't worked, conditions like erectile dysfunction and COVID-19 are common enough that there’s a financial incentive to keep companies looking for treatments.
But for a disease like the one that struck Bertrand and only about a dozen others worldwide, there are no other options. For patients with extremely rare diseases, repurposing existing drugs may be their only hope.
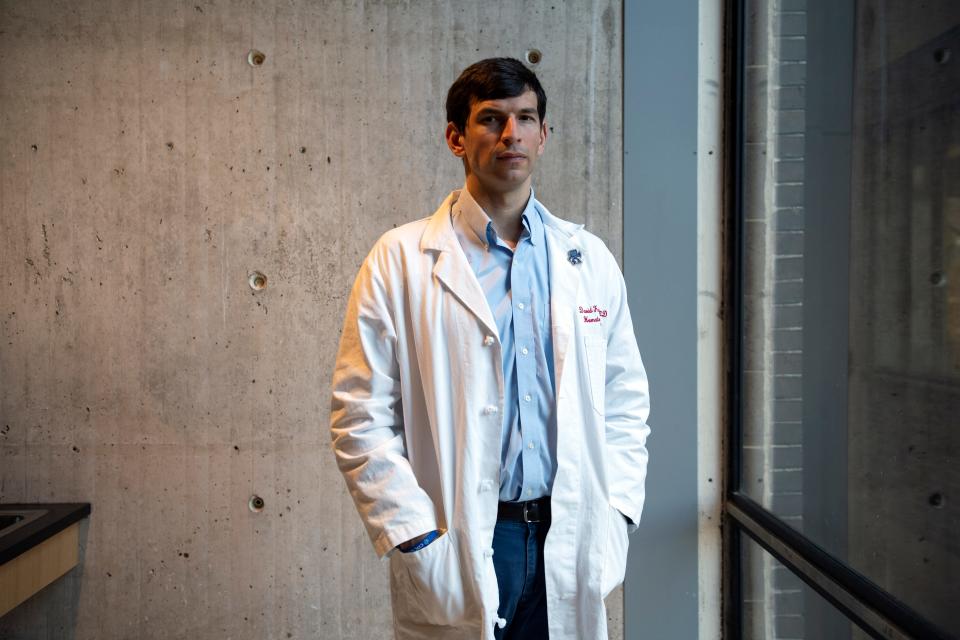
Dr. David Fajgenbaum is building on that hope.
Eight years ago, he repurposed a kidney transplant drug to save his own life.
“When I was so sick and running out of time, I knew I couldn’t develop a new drug, but I knew that there were 2,500 drugs already approved," said Fajgenbaum, who has a lethal autoimmune disease called Castleman. "It was my only chance.”
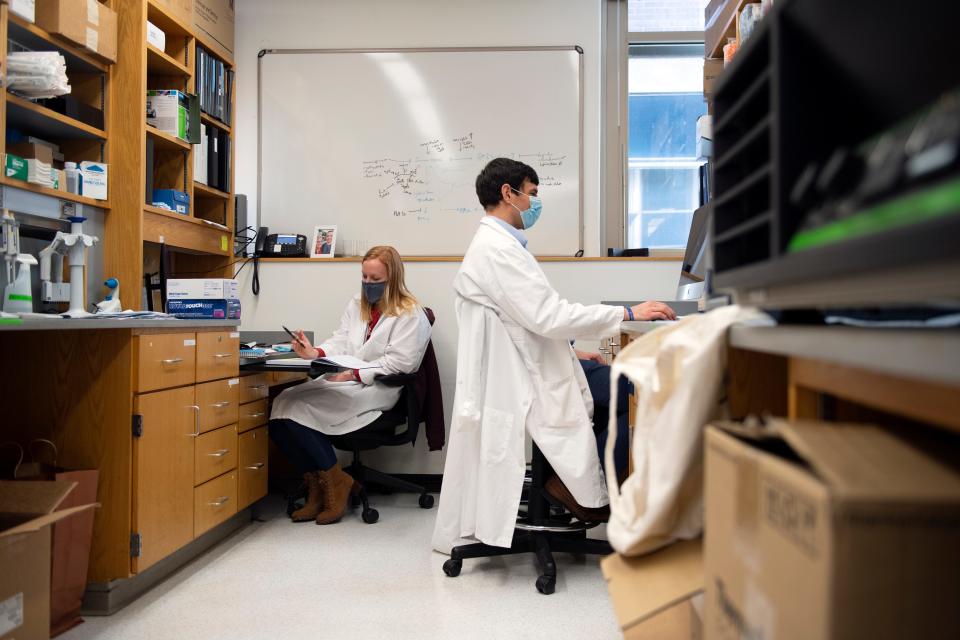
Now an assistant professor and associate director of the University of Pennsylvania's Orphan Disease Center, Fajgenbaum is trying to make the process of repurposing drugs easier.
“How many other patients can benefit?” he asked himself after he realized his own treatment was working. “Can this process be scaled?”
Might, Fajgenbaum and a small number of others are trying to add structure to the process and make the path to find an effective treatment less dependent on sheer chance.
Rare diseases may affect only a small number of people each – by definition in the U.S., fewer than 200,000. But that adds up to about 1 in 10 people, and only about 5% of these diseases have an approved treatment.
For many, drugs may already exist for other diseases that could help – if they can find them.
Fajgenbaum said he's motivated by the question: “What can we do to get these things that are usually found by luck to actually occur?”
Finding answers at the drugstore
When he realized his original treatment wasn't helping him, Fajgenbaum was in medical school with a girlfriend he wanted to marry.
Like him, about two-thirds of the 30,000 Castleman patients in the United States aren't successfully treated with approved therapies, and only 65% of patients with his subtype survive at least five years past their diagnosis.
Fajgenbaum didn't like those odds.
He decided to use his medical training to track a slew of his own biological metrics, including his immune system activation as he recovered, stabilized and descended into the next Castleman crisis.
The first sign of decline appeared to be an activation of T cells, the soldiers of the immune system, as well as production of a protein called VEGF, which promotes blood vessel growth. Sirolimus, a drug used to prevent organ rejection after a kidney transplant, blocks both.
With support from his doctor, Fajgenbaum began treatment. Seven and a half healthy years later, he's married with a toddler and a newborn, has written a book, "Chasing My Cure," about his experiences, and now has the means to help others do what he did.
“Sirolimus is in every single drugstore in the country,” he said, but no one knew it could work. “How many more are there like this?”
Fajgenbaum, now 36, was lucky. The drug he needed was off-patent and cheap enough that his insurance company agreed to cover it.
But in many cases, insurers want more proof before forking over thousands or tens of thousands of dollars a year for therapy. Clinical trials offer that proof but typically run into tens or hundreds of millions of dollars.
Companies aren't willing to make those investments unless they have some hope of recouping them, which is hard to do with a small patient population.
If more money were available for clinical trials or a few small changes could allow a patent to be extended without expensive trials, the incentives might shift. More drugs might be repurposed, Fajgenbaum said.
"When you think about these drugs, they've already been shown safe, effective for something and are at your neighborhood pharmacy," he said. "If you can make that link to another disease, you can change lives."
Bridging the gaps
Cures within Reach, a Chicago nonprofit, has been funding drug repurposing research since 2008.
The organization is financing 34 clinical trials, 40% of which are in rare diseases, said president and CEO Barbara Goodman.
While many in the drug development world think only new drugs can be innovative, "we think it's incredibly innovative to look at things that are already safe and effective and find out how many other ways we can test them in diseases and issues that don't have options," Goodman said.
Cures within Reach helps bridge the gap between an interesting laboratory finding and the need to prove it has enough promise by testing it in a small number of people.
At the University of Alabama at Birmingham, where Might directs the Hugh Kaul Precision Medicine Institute, he has designed a step-by-step process for patients called the Algorithm for Precision Medicine.
Analysts at the institute serve as biomedical research advisers to patients or foundations and help identify new uses for existing therapies.
Meanwhile at Penn, Fajgenbaum is trying to systematize the process of identifying approved drugs that might help those with rare diseases and overcoming at least the first hurdles for testing them in people. As he describes it, he’s helping “build out a map of the steps” needed to repurpose a drug and give rare disease groups a path forward.
"The first step is seeing what does the road look like," he said.
A researcher on his team recently surveyed 190 rare-disease organizations, asking questions about drug repurposing. While 75% said they were interested, just a small fraction were actually doing it. Fajgenbaum and his colleagues are trying to figure out how to change that.
He fantasizes about having a repository – a library – where people could look up the functions of different drugs and match them to their needs. Missing a key protein? Here’s a drug that happens to turn up production of that same protein. Wondering if a drug has a specific effect?
“There’s no group tasked with finding those things and shepherding them forward,” he said. “If it turns out not to be effective, let’s take it off the list.”
Finding needles in haystacks
To identify potential drugs, Fajgenbaum’s team has taken blood samples from about 100 patients with the same disease, measured about 1,500 proteins in each sample and looked for patterns.

Might’s team uses computer technology to scour millions of published papers written about therapies, looking for references to other effects the drug might have or similarities that might appear between symptoms and effective treatments.
Once the target drug is identified, it has to be tested further to make sure it is safe and does what the patients want it to do.
Might's UAB colleagues can model a patient's exact genetics as a worm or a zebrafish, and then use this to test existing drugs to see if they reverse symptoms.
They are also hoping to make use of the mRNA technology used in COVID-19 vaccines to develop easily customizable therapies for individual patients and small groups of patients with rare diseases.
But drugs don't always act in people like they do in a lab dish.
The controversial drug ivermectin, for instance, looked like a promising treatment for COVID-19 in a lab model but hasn’t been shown broadly effective in the real world.
Even treatments with plausible reasons to work don’t always do so. Convalescent plasma, taken from the blood of recovering patients and used to combat other diseases, like Ebola, seemed promising against COVID-19. But immune cells in the blood of recovered COVID-19 patients don’t confer the same disease-fighting ability, extensive studies during the past year have shown.
Testing has its challenges, too. Might had to find others around the world who shared Bertrand's NGLY1 gene mutation so he could run a clinical trial to persuade a drug company to tailor a concentrated version of Prevacid for these kids. (The collaboration for NGLY1 therapeutics has now moved well beyond "next-gen Prevacid," he noted.)
Fajgenbaum took a “Hail Mary” pass using himself as his own guinea pig in testing a drug used in kidney transplant patients to try to treat his own Castleman disease. Such experiments are worthwhile only when someone’s life is at risk. “There’s no way you’d use it if you had other drugs,” he said.
COVID-19 a test case
While looking for options for people with rare diseases, Fajgenbaum's group has also taken on repurposing drugs to treat COVID-19.
The nearly 2-year-old program, called CORONA, has tracked more than 800 drugs administered during the pandemic to identify those that might have the biggest benefit against COVID-19. The algorithm systematically identifies the most promising treatments, which can then be tested in large clinical trials.
Might said COVID-19 also helped speed up work needed to treat rare disease therapies, by proving the efficiency of the pathway for repurposing drugs. “In some ways it’s been a way to test-pilot the entire process all in one go,” he said.
But funding to test these new uses was in short supply as the government and corporations focus largely on vaccines.
"It seems like the vaccine race sucked all the oxygen out of the room early on for therapies, even though it's clear that novel and repurposed treatments are essential tools for saving life as the pandemic drags on," Might said.

Programs like his could have made a difference for more patients if they'd been financed earlier, he said. “Willingness to fund was the key.”
Timing is another lesson Fajgenbaum said he learned from COVID-19. A drug that didn’t help him when he was on death’s door might have helped earlier in his disease course.
Another patient with Castleman had been in the hospital for a year as doctors tried her on every conceivable drug. One of Fajgenbaum’s studies suggested a cancer drug might work in some people with the disease. She started on it in summer 2020 and was able to leave the hospital a few months later. Another patient dying of Castleman’s in Vancouver tried the same drug and also responded well.
These anecdotes don't add up to provable conclusions, but they may be enough to interest a company in making a targeted version of the drug for Castleman patients, Fajgenbaum said.
Such victories propel him and others in this work.
“There are all these pots of gold at the end of the rainbow,” Fajgenbaum said. “We just have to find them."
Contact Karen Weintraub at kweintraub@usatoday.com.
Health and patient safety coverage at USA TODAY is made possible in part by a grant from the Masimo Foundation for Ethics, Innovation and Competition in Healthcare. The Masimo Foundation does not provide editorial input.
This article originally appeared on USA TODAY: Repurposing approved drugs gives hope for treatment of rare diseases

